According to ScienceAlert, researchers from King’s College London have discovered that sections of DNA previously dismissed as ‘junk’ can be recruited to fight drug-resistant blood cancers, particularly myelodysplastic syndrome and chronic lymphocytic leukemia. The international team found that mutations in ASXL1 and EXH2 genes, common in these cancers, reactivate transposable elements that stress cancer cells and make them dependent on PARP repair proteins. Using mouse models and human cancer cells, they demonstrated that PARP-blocking drugs effectively kill these cancer cells while largely sparing healthy ones. The research, published in Blood, offers a novel approach to treating hard-to-target cancers by leveraging existing drugs in new ways against previously overlooked genetic elements.
The Junk DNA Revolution
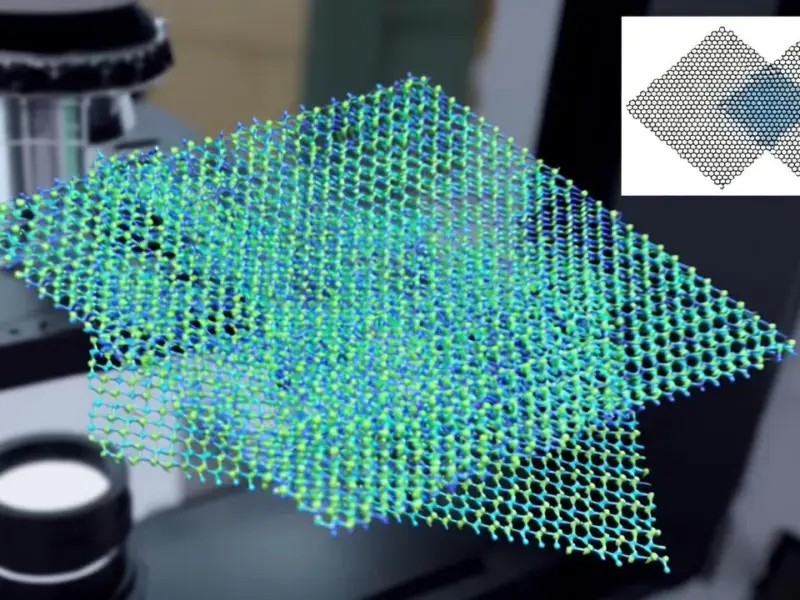
This discovery represents the latest chapter in a fundamental rethinking of human genetics that’s been unfolding for decades. When the human genome was first sequenced, scientists were surprised to find that only about 2% of our DNA actually codes for proteins. The remaining 98% was initially dismissed as evolutionary debris or ‘junk’ DNA with no functional purpose. We now understand this was a profound misunderstanding. These non-coding regions, including transposable elements that make up nearly half our genome, serve as sophisticated regulatory systems that control when and where genes are expressed. The King’s College research demonstrates that cancer cells inadvertently activate these ancient genetic elements as part of their uncontrolled growth, creating a vulnerability that can be exploited.
Beyond Blood Cancers
While the immediate focus is on specific blood cancers, the implications extend much further. PARP inhibitors like olaparib and rucaparib are already FDA-approved for treating ovarian, breast, and pancreatic cancers with BRCA mutations, but their mechanism has been understood differently. This research suggests we may have been underestimating how these drugs work and potentially missing broader applications. The King’s College announcement indicates the team believes their findings apply to other cancer types, which could significantly expand the patient population that might benefit from existing PARP inhibitor therapies. This represents a faster path to clinical application since safety profiles for these drugs are already established.
Transforming Treatment for Resistant Cancers
For patients with chronic lymphocytic leukemia and similar conditions that develop treatment resistance, this approach offers hope where options are limited. Traditional cancer therapies target specific proteins produced by mutated genes, but when those genes stop producing targetable proteins, treatment options dwindle. By instead targeting the cellular stress response mechanisms that cancer cells become dependent on, researchers have found a way to attack cancers that have evolved resistance to conventional treatments. This synthetic lethality approach—where two genetic vulnerabilities combine to kill cancer cells while sparing healthy ones—represents a smarter way to fight cancer evolution.
The Road to Clinical Application
Despite the excitement, significant challenges remain before this approach becomes standard care. The research is still in preclinical stages, primarily using cell lines and animal models. Human trials will need to validate both efficacy and safety, particularly regarding potential off-target effects on healthy cells. Additionally, identifying which patients will benefit requires developing reliable biomarkers to detect when cancers have activated these transposable elements. Previous research published in Cancer Discovery has shown similar mechanisms in other contexts, suggesting this isn’t an isolated phenomenon, but translating these findings into predictable clinical outcomes requires careful validation across diverse patient populations.
Redefining Genetic Medicine
This discovery continues the trend of finding function in what we once considered genetic ‘dark matter.’ Beyond cancer treatment, understanding how transposable elements influence gene regulation, immune responses, and cellular stress could impact how we approach genetic diseases, aging, and even neurological conditions. The fact that nearly half our genome consists of these mobile elements suggests we’re only beginning to understand their role in health and disease. As sequencing technologies advance and computational methods improve, we’re likely to discover more ways that this ‘junk’ DNA serves as both a vulnerability in disease and a potential resource for innovative treatments across multiple medical disciplines.